
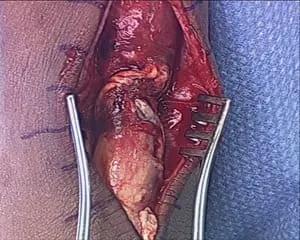
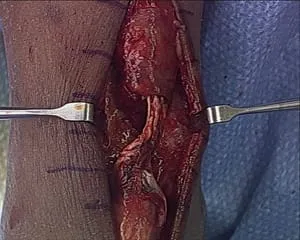
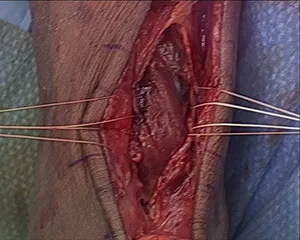
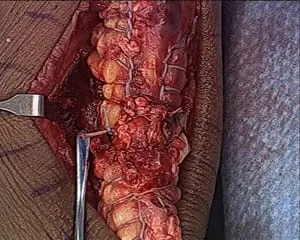
Below are intra-operative pictures of an Achilles tendon repair. The image to the left is a tendon that has been repaired to be reattached with sutures in place and tendon cleaned of the diseased tendon. The picture to the right is the tendon re-approximated with sutures tied.


ACHILLES TENDON RUPTURE
By: Robert H. Sheinberg, D.P.M., F.A.C.F.A.S., D.A.B.F.A.S.
Achilles tendon ruptures are the most common tendon ruptures of the lower extremity. They can occur at any age, but are most common in the third to fifth decade. There is a significant male preponderance. The classic description is the "weekend warrior" athlete.
Anatomy
The Achilles tendon is the common tendon of the gastrocnemius and soleus muscles and provides their attachment to the calcaneus. The soleus muscle arises from the posterior tibia while the gastrocnemius arises from the posterior distal femur. This allows the gastrocnemius to be effective with an extended knee and the soleus to be more effective with a flexed knee.
The tendons from both muscles coalesce just distal to the musculotendinous junction to form the Achilles tendon. The tendon has a relative avascular portion 2-6 cm above the insertion. The tendon also rotates approximately 90 degrees during its course, with the gastrocnemius fibers being more lateral. The tendon inserts upon the posterior calcaneus primarily along the posterior tuberosity with slightly more medial than lateral extension.
Pathogenesis
A relatively hypovascular area exists approximately 2-6 cm above the insertion into the calcaneus. This hypovascularity has been implicated in disorders of the tendon. Age-dependent changes in collagen cross-linking result in increased stiffness and loss of viscoelasticity, which may predispose the tendon to rupture. Mechanisms associated with ruptures include suddenly forced dorsiflexion of the ankle (eccentric contraction of the gastrocnemius and soleus), pushing off with the weight-bearing forefoot while extending the knee, and laceration or a direct blow to the contracted tendon.
Classification
Achilles tendon ruptures are partial or complete. Ruptures can also be divided into acute traumatic ruptures, chronic ruptures, or chronic attritional ruptures. However, ruptures are often due to a combination of age-related attrition and an acute traumatic incident.
Patient History and Physical Findings
The patient with Achilles tendon rupture presents with pain in the area of the Achilles tendon. The pain of an acute rupture is often described as an intense burning sensation or sharp stabbing pain. Patients may hear an audible pop after an eccentric muscle contraction or be pushing off; they usually describe a feeling of being kicked, hit, or shot in the heel. A small percentage of patients will have prodromal symptoms. In the presence of a complete tear, patients will experience significant ankle plantar flexion weakness. However, many patients continue to be able to actively plantarflex the ankle using accessory muscles. This may confound some examiners and result in a missed diagnosis.
Physical findings include a visible soft-tissue depression in the posterior ankle on observation. The tendon defect can often be palpated along the posterior leg and ankle. Patients may be unable to walk or walk only with a limp secondary to weak or absent push-off. The absence of active plantarflexion is often expected, but many patients effectively recruit other muscles to plantarflex against manual testing. However, they are rarely able to perform a single leg heel raise. With the patient in the prone position and the knees flexed, the Thompson squeeze test is executed by squeezing the calf muscle and observing the presence or absence of resultant ankle plantarflexion and comparing with the contralateral side. Another helpful test is to observe the resting position of the ankle compared to the unaffected side with the patient prone and the knees flexed to 90 degrees.
Imaging and Diagnostic Studies
Radiographs are rarely diagnostic. They may be warranted in cases of extremely distal ruptures when avulsion of part of the calcaneus needs to be ruled out. Ultrasound and MRI can accurately demonstrate ruptures but are rarely necessary with classic clinical findings. These studies may be helpful when the diagnosis is unclear.
Treatment
Treatment for acute Achilles tendon ruptures can be operative or non-operative and much controversy exists. Historically, the pendulum swung towards operative treatment (especially of younger, healthier patients) because of the much lower reported re-rupture rate (2% for surgical and 11-30% for non-surgical), accepting the trade-off of potential wound complications.
Non-operative Treatment
Conservative treatment varies and classically involved casting in a long leg cast with the knee flexed and ankle in equinus (2-3 weeks), then short leg casting (8 weeks). Nonweightbearing was typically recommended initially (the first 6 weeks).
More recent approaches include functional bracing with immediate weight-bearing. These more aggressive protocols describe immediate full weight-bearing in a functional brace or pre-fabricated boot. Patients are started with the ankle in up to 45 degrees of plantarflexion, which is gradually decreased to neutral over 6 to 12 weeks. They often perform active plantarflexion exercises with restricted dorsiflexion during that time, then graduate to more aggressive strengthening protocols.
Operative Treatment
At South Florida Institute of Sports Medicine, the Foot and Ankle Surgeons prefer open operative repair. Depending on the existing tendon condition and timing of repair, cast immobilization varies from 2-6 weeks. Weight-bearing begins at 4-6 weeks and intensive physical therapy follows with a Cam Walker transitioning back to shoe gear.
Intraop pic of Achilles ruptures prior to repair. There is a 1-cm gap between the tendon ends. The white tendon on the left is called the plantaris. Due to this tendon being intact, the Achilles didn't retract much after the rupture.

This is a pic with the sutures on both ends of the rupture prior to be tied.

These are final pics of the repair with the tendon edges tightened before after the suture ends are cut.>


Krackow suture of both Achilles rupture stumps.


Rupture is Repaired and the FHL muscle can be seen as one with the Achilles to allow increased blood flow for healing.


Intraop picture of Achilles tendon rupture. We have made a posterior fasciotomy to visualize the FDL muscle. We have 4 sutures in the center of the pic that is in the muscle belly. We tie these sutures on the pic of the tendon after the repair. This gives a better blood supply to the repair site.
Pic of Rupture. The white tendon to the left is called the plantaris tendon. It doesn't give any tension to the Achilles or repair.

Krackow suture technique to lock the 2 ends of the repair site to decrease tension to the repair.



Pics of the complete repair



Achilles tear

Krackow suture technique on both sides of the Achilles tendon that locks the tendon on both sides of the Achilles to decrease tension at the repair site.

Reapproximation of the ruptured ends of the Achilles tendon.

Completed repair of the achilles tendon.

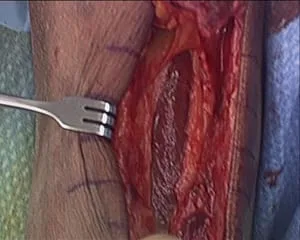
Series of pics during Achilles tendon rupture repair with posterior fasciotomy and FHL muscle transposition to increase vascularity to the repair site (below).
The rupture ends are at the top and bottom of the pic.

The window is made in the fascia between the Achilles and FHL muscle (muscle that moves the big toe down). We pass suture into the muscle and this can be seen in the fingers on the left and right of the pic.

We have sutured the ends of the Achilles tear and these will be sutured together to repair the tear.



The tendon is tied together and the sutures placed in the FHL muscle are tied around the tendon to tranpose the muscle to the tendon repair to increase vascularization to the tendon and promote better healing.


Below are the pics of the Krackow suture technique we use to repair the proximal and distal repair stumps together. We interweave a non-absorbable suture through each rupture end and then tie them together to reapproximate the tendon.


We have repaired the Achilles and are preparing to transpose the FHL muscle to the repair site to increase vascularity. The four sets of white suture can be seen on the sides of the Achilles.


Pic after complete repair with muscle transposition.

The instrument is identifying the FHL muscle as it is transposed to the repair site to increase vascularity.

Repair of traumatic Achilles tendon rupture with Krackow suture technique and FHL muscle transposition.
View of the rupture.
View of the posterior fasciotomy and exposed FHL muscle to increase vascularity to the repair.
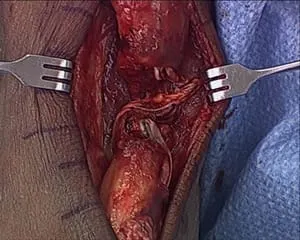
We have placed absorbable suture through the muscle belly to later transpose to the front of the repair.
Achilles Rupture has been repaired with a Krackow technique and the absorbable suture can be visualized from each side of the Achilles prior to suturing.

Pictured below is an image of a torn Achilles tendon. The ends are frayed because this is a result of a chronic degenerative process similar to when a rope startes to wear out and then finally gives out.

This is the same tendon after surgical repair.

Another case of a torn Achilles tendon as a result of chronic degernation of the tendon fibers.

.
This is the tendon being repaired with suture using a technique called a Krachow stitch.

This is an image of the repaired tendon

Intraoperative picture of an avulsion of the Achilles off the calcaneus.


Below the Achilles is pulled through a trough in the heel bone to re-anchor it down).

Pic below of an avulsion of the Achilles off the heel bone prior to repair and re-anchor through the heel.

Achilles rupture intraoperatively before and after repair.


Series of intraop pics of an Achilles rupture with part of posterior calcaneus still attached. This was a 17-year-old competitive cheerleader who jumped and injured her heel.
The Achilles is torn off of the back of the calcaneus and a portion of the heel is still attached to the Achilles. The back of the heel bone is the rounded yellowish bone at the bottom of the incision site.

Nonabsorbable suture has been weaved through the Achilles to repair it back to the back of the calcaneus.

A trough is made in the calcaneus to allow the tendon to have ingrowth at its reattachment site in the posterior heel.

The suture from the Achilles is placed through two small drill holes in the trough and out the bottom of the heel bone.



The Achilles is tensioned down into the trough and reattached to the calcaneus.


Intraop pic of Achilles rupture prior to repair. There is a 1-cm gap between the tendon ends. The white tendon on the left is called the Plantaris. Due to this tendon being intact, the Achilles didn't retract much after the rupture.

This is a pic with the sutures on both ends of the rupture prior to be tied.

These are final pics of the repair with the tendon edges tightened before and after the suture ends are cut.


Intraoperative pics of Achilles tendon rupture before and after repair.


Intraop pic of Achilles rupture before and after repair.



